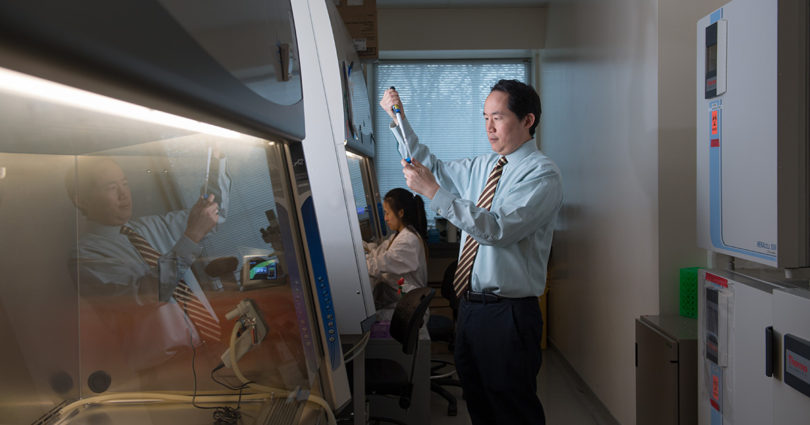
Dr. Stanley Liu is a radiation oncologist at Sunnybrook’s Odette Cancer Centre and a researcher in Biological Sciences at Sunnybrook Research Institute.
Dr. Liu’s lab was involved in a large, multisite study published today in Nature Genetics.
The study carefully examined more than 8,000 tumours at the genetic level to help better understand the effect of low oxygen (hypoxia) on cancer.
Dr. Liu couples his roles as a clinician and a biological scientist in the hope of unmasking some of the mysteries of cancer to help come up with better, more tailored treatments for his patients.
What’s this hypoxia study all about? What are the key take-aways?
It’s long been known that tumours thrive in low-oxygen environments. Low oxygen can make tumours resistant to treatments and more likely to spread to other sites in the body. Despite being a well-known cause of treatment resistance and cancer spread, the impact of low oxygen, known as hypoxia, on tumour cells has been poorly understood.
This is an important large-scale study that involved collaborators across many locations and analyzed the genes from a broad range of tumour types. It confirms what’s been known about low oxygen tumours and helps us further understand that because of hypoxia, there’s a loss of tumour suppressor genes, an activation of oncogenes (genes with the potential to cause cancer) and many alterations in messenger RNA and microRNA that control protein production. Understanding these common traits will be an important step forward in the personalization of cancer treatment.
We can use these genetic markers and information to make a collective “score” for a tumour. That score may help us determine who might benefit from a hypoxia-targeting agent. These drugs have been around for awhile, but giving them to everyone doesn’t make sense (they can have lots of side effects and only benefit certain types of tumours.)
We know that when we use radiation to treat tumours, we can generally have great success. But if that tumour is hypoxic, the radiation treatments may not work as well. For those patients, there could be a role for these hypoxia-targeting agents. It’s really a step toward more personalized treatments.
A lot of centres around the world were involved in this study. Why is that important?
Genomics is complex. It needs a large number of samples from many different centres so that we can compile enough information.
It’s not something that one research centre can do in isolation. One genetic test isn’t going to come up with the answer to help treat all cancers. It’s looking at what we know and using a number of tests in collaboration to come up with the best ways to personalize treatment for a patient’s tumour.
Each and every tumour is unique. So we will need to use pathology, combined with information about a tumour’s genetic and protein profile, so that we can begin to really tailor treatments for each patient.
What do you want people to know about genetics and genetic research?
More people is more power — power being information. Some patients may be hesitant to participate in this kind of research because the thought of their tumour cells or information being stored doesn’t sit well. But every person matters in this kind of research. Every tumour is unique and the more samples we have, the better understanding we can have, and the better, more precise treatments we can offer. Without patient samples, we can’t personalize treatments. Every patient who gives a sample is making a difference. It’s so valuable to science and to patient care now and in the future. We can go back to the data; we can go back to the samples; we can use this information to help develop and optimize new tests and treatment technologies.
There’s a real challenge for this kind of research because of the costs involved, limited research funding, and the length of time it takes to build a meaningful database, in terms of patient numbers and clinical follow up.
What’s next for you?
I’m involved with a multi-site project now that is examining aggressive prostate cancer at the DNA, RNA, microRNA and protein level so that we can build a database of these types of tumours. We will then compare the genetic profiles with patient outcomes and see what types are most aggressive and what genetic markers those cancers have.
How does being a clinician impact your research?
My work as a radiation oncologist helps me define clinical problems, and guide the important questions that need answers.
I see the realities of cancer. Some patients do really well. But there are still many patients who don’t respond well to treatment and who do poorly.
As a scientist, I could look at the data, and the genes, and the graphs and say, “Look! It’s so clear!”
But then in the clinic, I look at my patient who is not responding to treatment, and I’m reminded that things don’t always work the way they do on charts and papers. That inspires me to keep up with this kind of research. There’s so much more to see and to understand.