When a Code Orange was called on Monday, April 23, the day of the Yonge St. van attack, Sunnybrook staff were prepared.
At 1:27 pm, a man drove a white rental van onto the sidewalk near the intersection of Yonge and Finch streets, deliberately hitting pedestrians. Ten people died and 15 were injured.
At 1:48 p.m., Sunnybrook issued a Code Orange, warning staff that victims of a mass casualty were on the way. Ten of the injured were taken to Sunnybrook’s campus on Bayview Avenue – less than 10 kilometres from the scene of the tragedy.
The victims started arriving seven minutes after the Code Orange was called, at 2:06 p.m. Here is how several Sunnybrook employees recall what happened on that day.
Miranda Lamb

Miranda been a nurse at Sunnybrook since 2005. She was the nurse in charge of the Emergency Department on the day of the van attack.
Has been a nurse at Sunnybrook since 2005. She was the nurse in charge of the Emergency Department on the day of the van attack.
I had agreed to trade a shift with a colleague that day, so I was in the Emergency Department (ED), in charge.
When the patients arrived they were all triaged, assessed by the trauma team and emergency staff and cared for in the ED or sent to the operating room or the intensive care unit.
You very quickly realize in a Code Orange that you cannot do everything yourself; you have to work as a team across all disciplines and departments. In the ED, we are the first ones who see patients coming into the hospital, but we had staff come from all over the hospital offering their help. Everybody had to stretch beyond their usual capacity. It was just remarkable in that way. We had one goal: to receive, stabilize and provide care for each patient – no matter what they needed.
I’ve always said that working in the ED is unique, and we sometimes see the people we work with more than our own families. So you need to be able to rely on each other to get through tough situations.
You also need to rely on your team after an event like this, to make sure that everybody is okay and feels supported. It was only after we cared for all of the patients that we could begin to appreciate the full extent of what had happened on Yonge Street, and what the impact would be for the families and patients.
We too were experiencing this event as mothers, fathers, sisters, brothers, Torontonians and caregivers. We all went in to do a job that day, but we’re all human.
Val Soper

Val has been a social worker in Sunnybrook’s Emergency Department since 2003.
I was in the Emergency Department (ED) when the Code Orange was called.
My social work colleagues from across the hospital were in contact with me immediately by phone, text and in-person to see how they could help. Along with emergency preparedness leaders, a decision was made to set up our Family Information and Support Centre quickly in the hospital’s auditorium. We knew family members and loved ones would be on their way soon.
The support centre was staffed by Social Work, Spiritual Care and Volunteer Resources. On that particular day, we also had other disciplines offering to help. Psychiatry was there, a music therapist, an occupational therapist, a geriatric nurse and others.
I spent most of my time in the ED and in communication with support centre staff once the centre was set up. The first thing I did was station two staff members at the ED entrance, as well as the hospital’s main door, to direct arriving family and friends to the support centre to start the process of locating their loved ones.
In the early evening, I moved from the ED to the support centre. At that time, many of the families had been registered, “matched” and reconnected with their loved ones, who were being treated in hospital, in intensive care or in surgery. At the end of the night, my job was to support those families who were still waiting for news. The last family was there until 2 a.m.
The Sunnybrook response was incredibly united. We all pulled together and worked as a team. Our emergency preparedness – all those Family Information and Support Centre meetings and mock exercises – helped on this very difficult day.
Dr. Fred Brenneman
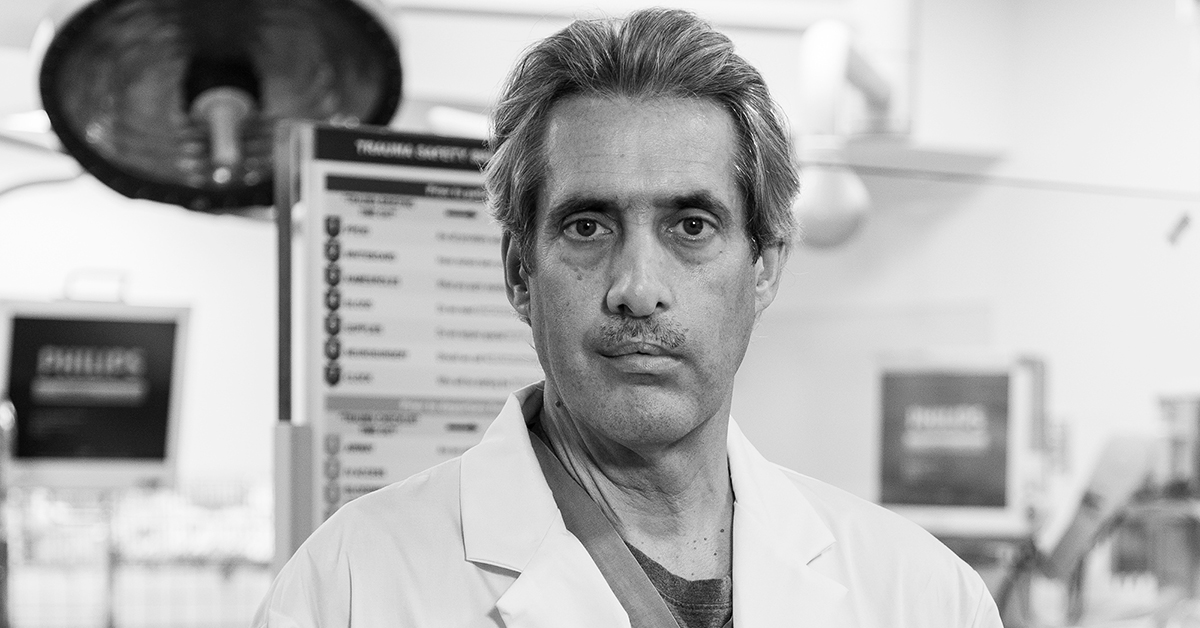
Dr. Brenneman is a trauma surgeon at Sunnybrook, where he’s worked for the past 23 years. He previously served as a medical director of the trauma program.
People were extremely keen to offer help and provide whatever they could regardless of what they were doing at the time, whether or not they were on call.
It happened at a time when the hospital was full with high bed occupancies. To the credit of those who manage beds and to the surrounding GTA hospitals that pitched in and offered to take some of our stable inpatients, we cleared enough Intensive Care Unit (ICU) beds and operating rooms to manage the surge.
We normally have one trauma team working per day, but with the Code Orange call, we very quickly had three teams assembled in the trauma bay looking after the patients.
I supervised the management of one patient until they were off to get a CT scan. Then,
I took another patient up to the operating room because I was the surgeon on call that day. By the time that operation was finished, our patients had their destinations allocated. Some of them were already in the operating room, some of them were in the angiography suite for imaging and treatment, and some were already in the ICU – so the process to treat everyone’s injuries happened pretty quickly. If you do what you need to do and trust your expertise and your training, then there’s no panic. I am very proud of the Sunnybrook team’s response.
Johnny Amatuzio

Johnny is the supervisor of security services at Sunnybrook, where he’s worked for a decade.
Because it was publicly broadcast that most of the injured were coming to Sunnybrook, we decided – for safety – to go on lockdown. What that does is restrict access to the Emergency Department (ED).
Our Security staff set up for crowd control. We made sure that the roadway to the ED was clear for multiple ambulances. When patients started arriving, we escorted the stretchers to the trauma bay.
My manager and I called everyone in our department. Several people came in early for their shifts and others came in on their day off.
Everyone in the hospital came together to make sure everything could be done to the best of our ability for all the patients and their families. My heart goes out to all those whose lives were changed by this tragedy.
Vanessa Flores

Vanessa is a respiratory therapist at Sunnybrook in the Intensive Care Unit (ICU).
The hospital team leaders started to gather the doctors in the Emergency Department (ED) to brief them about the Code Orange situation.
They said a van had hit multiple pedestrians and there were many patients who needed critical care. I immediately called our department and spoke with a senior staff member and said we needed all of the transport ventilators brought downstairs to the ED.
I headed upstairs to help grab equipment and by the time I made it back downstairs, there were already patients coming into the trauma bay. I moved to a bedside – making sure anaesthesia was there, preparing my monitors and coming up with a game plan with the team.
We called in extra staff and thankfully three extra respiratory therapists came in.
A critically injured patient arrived requiring stabilization and admission to the intensive care unit. I was with that patient for two-and-a-half hours.
Everybody stepped into their role and focused on what they would normally do, but as if in fast-forward. I was thinking, ‘how can I get this patient stable, move them to a scanner and get them a bed?’
Eventually, once all of the initial activity was over, we had an opportunity to sit and kind of calm down because when you’re working with your patient, you’re so focused that you can lose track of time.
We had multiple debriefs afterwards. At the debrief for the respiratory therapists, hospital leadership said, “We’re here to listen to you. What would you like to talk to us about?” It was a very open and safe discussion. We felt we could just be very truthful about how we were feeling without judgment, which was fantastic.
Dr. Oskar Singer

Dr. Singer has been an anesthetist at Sunnybrook for five years.
On a normal day, we have one anesthetist who’s the main operating room co-ordinator. Anesthetists carry phones and relay with the nursing team and the surgical team, making plans for the day. They determine which emergency case should go into the operating room next.
My colleague, Dr. Paul McHardy, was in that role when the Code Orange was called, so I was able to help coordinate trauma patients downstairs in the trauma bay.
I grabbed a phone and ran downstairs. As each patient was triaged, assessed and a plan was made, I’d immediately call Dr. McHardy and give him a perspective on what the patient needed. From the moment that patients started coming in, the atmosphere was intense but controlled.
Patients who were coming in after the trauma bay was full were triaged to available Emergency Department (ED) beds. Porters moved patients in the ED who were doing well enough to make space for new, more seriously injured patients.
We sent patients with life-threatening injuries immediately to the operating room. Others were stabilized and sent with teams to CT scanners to determine what kind of internal injuries had occurred.
This was definitely the most significant, large-scale incident that I’ve been part of. I think one of the interesting things that happens is you automatically fall back on your training.
Above all else, you’re doing everything for the patient before you focus on how you actually feel. For me, that happened when I got home that night and had some time to reflect on the gravity of what we’d just gone through, the number of lives that were affected and the permanent changes that happened to so many families.
A few things stand out about that day, including how well everyone interacted and came together at such a dire time. One example is how quickly the Environmental Services staff were able to turn over the trauma bays in between patients to ensure the most efficient care.
The other was how quiet the trauma bays were; obviously there was the noise of action and people communicating with each other, but it wasn’t as chaotic as you’d think it would be. Everyone was ready to go.
Adonis Lopez

Adonis worked as a patient service partner at Sunnybrook, providing personal support services to patients and their health-care teams for 14 years.
The Code Orange was called one hour into my shift. One of my first tasks was to deliver stretchers and wheelchairs to the Emergency Department.
After that, I was asked to help set up the Family Information Support Centre in the auditorium, a place where family and loved ones could gather to receive news and emotional support. We couldn’t really anticipate how many people were coming, so we set up as many private areas as we could with the equipment we had. We thought of other things we would need, like water, hand sanitizer, pens, tissue boxes, and then we’d go out and get them.
Then I was stationed at one of the hospital’s entrances, so when families arrived we could walk them to the Support Centre.
The Emergency Department was in lockdown, so families entered through the other hospital entrances. I approached those who looked lost or concerned and asked if they needed help.
I’ve worked in the Critical Care Unit and in Same Day Surgery, and I understand that Sunnybrook is a trauma centre, but I didn’t actually realize how serious the incident was until afterwards, when we had our debrief meetings. That’s when it hit me. I hope that the little things I did helped and that a lot of the little things other people did helped, too.
Dr. Dan Cass

Dr. Cass is the executive vice-president and chief medical executive of Sunnybrook.
I don’t think there was anyone at Sunnybrook who wasn’t in some way part of the Code Orange response.
The obvious ones were the staff in the Emergency Department – the trauma team leaders, nurses and respiratory therapists – as well as those in the Critical Care units, the operating rooms and Medical Imaging. But as soon as this happened, all of the teams from the medicine units began going down to the Emergency Department and bringing admitted patients up to the wards. Even if teams weren’t part of the direct response to the Code Orange, they were part of making room for someone else.
It’s also important to recognize the group that set up and staffed the Family Information Support Centre (FISC) to support families, gather information and help connect victims from the incident with family members and loved ones.
I think all of us in Toronto were affected. This was an event that happened in our home, and it’s an emotionally jarring thing for anyone to have to come to terms with, let alone being personally involved.
Aileen Ho

Aileen is a physiotherapist in the burns and trauma unit at St. John’s Rehab, which has been part of Sunnybrook since 2012.
I’ve often said that I live in a small bubble of only a one-kilometre radius. I live about a block from Yonge and Finch. I went to school in this area. lean walk to work, bike to work – I’m that close.
My three-year-old daughter’s daycare is pretty close to Yonge and Finch. That day, I was really concerned about her because the kids go out for walks in the neighbourhood a lot. Was she safe, did they go into lockdown? I worried she might have seen something, but luckily, she didn’t.
I had just come back from maternity leave [Ho also has a one-year-old daughter] on the day of the incident. News was spreading about a big, multiple fatality happening really close to us. (St. John’s Rehab is located less than two kilometers from the scene.)
Many of us who work at St. John’s Rehab were thinking that a lot of the victims would have gone to Sunnybrook due to the proximity of the incident and that, eventually, we would be seeing them in our unit. In preparation, we had team meetings to discuss how to best prepare for caring for these patients.
They started coming in to St. John’s Rehab soon after and our team went to work.
So often, it’s when they’re in physiotherapy that trauma patients really open up. We’re constants in their lives when they’re in rehab because we see them every day and a strong rapport is built. I think a lot of us love our jobs because of those relationships and the difference we make in our patients’ lives.
I’m always excited when someone takes their first step because sometimes it can take months to get to that point after an injury. Even just little changes – like when they no longer have a cast or splint, or being able to put a little weight on their legs – it’s a big celebration. Every little change is a big change.
Just sharing the joy with them is wonderful. That’s what you come to work for every day.
Photography by Kevin Van Paassen
Our thoughts — and our hearts — continue to be with the victims and families of the Toronto van attack and Danforth shooting.